There are over 80 different sleep disorders, each troubling in its own way. The average person could maybe name a handful of these sleep disorders, but there are some that are often misunderstood or not known by the general public. One of these little-known sleep disorders is called cataplexy. Even medical professionals and sleep experts can misunderstand the disorder, leading to misdiagnosis or frustration on behalf of the patient.
Cataplexy is associated with narcolepsy but with some key differences. Narcolepsy is more well-known as it is often portrayed on television or in movies with a person suddenly falling asleep or becoming incredibly drowsy without warning. With narcolepsy, a person can lose consciousness as they fall asleep; however, with cataplexy, a person loses muscle control while staying awake.
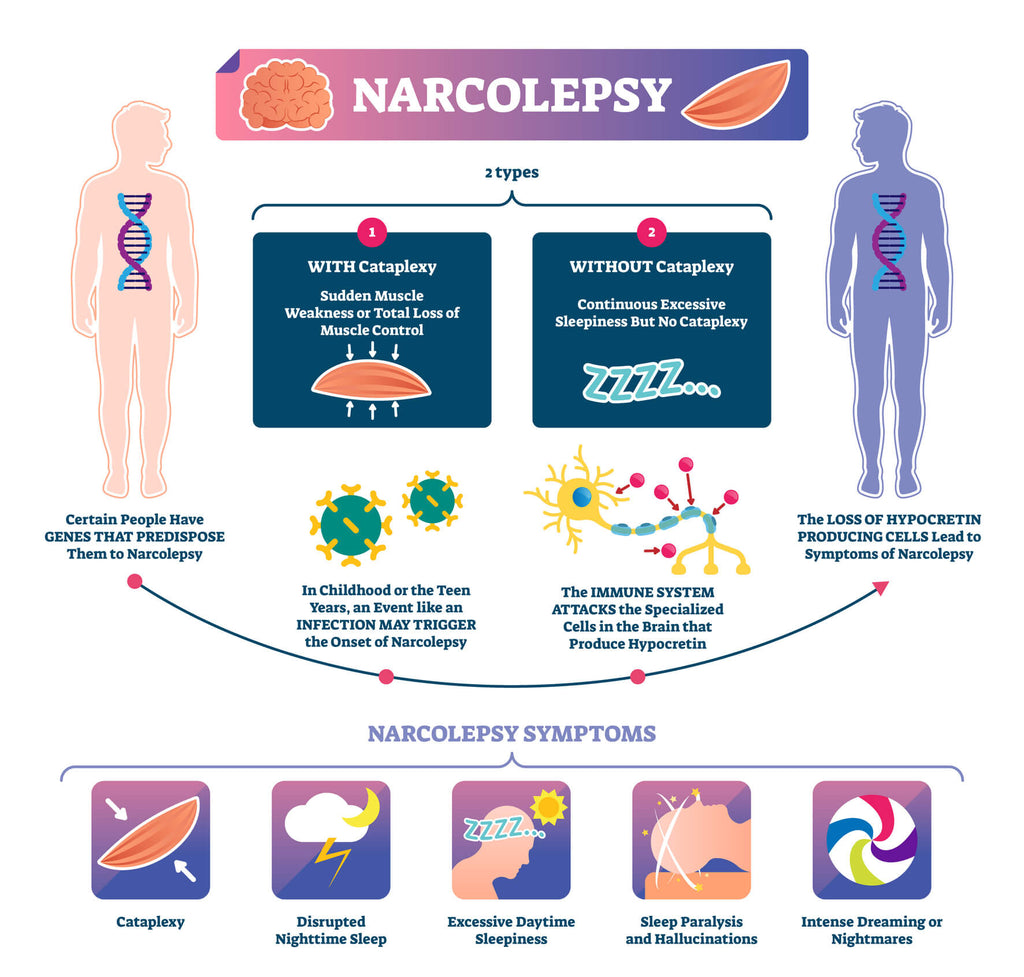
Someone who has cataplexy may be diagnosed with narcolepsy, but a narcolepsy diagnosis does not mean a person has cataplexy. A cataplexy diagnosis may or may not be associated with narcolepsy, or it could be a side effect of meditation or a result of a genetic disease. Diseases and health conditions such as stroke, multiple sclerosis, head injury, or excessive daytime sleepiness (EDS) can also trigger cataplexy.
Non-narcoleptic cataplexy is when cataplexy is related to a rare genetic disease or medication. Some genetic conditions that can cause cataplexy include Norrie disease, Angelman Syndrome, Niemann-Pick type C Disease, and Prader-Willi Syndrome. Medications that can cause non-narcoleptic cataplexy include clozapine, gamma-hydroxybutyrate, and lamotrigine. As you can see, there are several potential causes which is why this sleep disorder is considered so complex!
Cataplexy is often linked to narcolepsy type 1 because both are thought to be the same form of muscle paralysis that occurs during REM sleep. As a result, both sleep disorders share similarities to sleep paralysis. Sleep paralysis would occur if you were sleeping soundly on your millet pillow and then woke up but couldn’t move your body. This sleep disorder often co-exists with narcolepsy and ties into the REM stage of sleep. Both cataplexy and sleep paralysis are believed to occur most frequently on the edge of sleep, meaning right before you fall asleep or as you wake up.
Symptoms of Cataplexy
The symptoms of cataplexy can vary in severity, and the disorder can appear at any stage of life. Typically, the disorder will first present between the ages of 7 and 25 but is not limited to this age group. Common symptoms include involuntary tongue movements, trouble speaking, drooping eyelids, facial twitching, jaw tremors, jaw drooping, and head tilting. More severe symptoms occur when voluntary muscles lose control, and an individual collapses.

When a person collapses due to a loss of voluntary muscle control, it is known as a cataplectic attack. The person will remain conscious and awake through the process, falling to the ground. Losing muscle control and falling to the ground poses many safety risks, as an individual could severely injure themself or hit their head. However, in many cases, a person will start to experience warning signs like twitching or difficulty speaking and can get themselves to a safe place or lie down to avoid potential injury during an attack.
These cataplectic attacks typically only last a short period of time, with a person gaining muscle control within 30 seconds to 2 minutes. In some cases, a person may only experience an attack once or twice in their life, but in more severe cases, it can happen multiple times each day.
Outcome of Cataplexy
Although the sleep order can feel devastating to a person experiencing regular episodes, there are no immediate health concerns because of it. Instead, the biggest threat to those living with cataplexy is an injury when a person loses muscle control. For example, falling while crossing the street or hitting their head on a concrete floor can cause severe outcomes.

Those living with cataplexy can suffer from sleep deprivation as well. This can cause additional health concerns such as depression, anxiety, obesity, diabetes, and cardiovascular disease. When the sleep disorder is left undiagnosed, and without treatment, it can be very concerning and stressful.
Because of the adherent risks of unexpectedly losing muscle control, those experiencing cataplexy symptoms should avoid driving or operating heavy machinery. The shortest attack could have deadly consequences for the driver and others on the road. As a result, an individual may have to make modifications to their life and field of work.
Causes of Cataplexy
Although complex and sometimes confusing, research has found that cataplexy is often triggered by intense emotions such as fear, excitement, stress, anger, and even laughter. The loss of muscle control could happen to their entire body or just to one side. Studies suggest this loss of control is linked to a decrease in neurons that produce a neuropeptide hormone called hypocretin. Hypocretin is a hormone that manages energy expenditure, appetite, arousal, and wakefulness. In 2010, one study found that this reduction in hypocretin was caused by an autoimmune response that led to antibody production that targeted and killed off hypocretin-producing neurons.

Diagnosing Cataplexy
Because the disorder is complex, it isn’t easy to diagnose and is considered quite rare. Although the exact prevalence isn’t known, research suggests that only about 10% of narcoleptic cases are cataplexy. When experiencing these troubling symptoms, a person will see their doctor. The individual will then undergo a series of tests to determine the cause.

Generally, a person will first participate in a sleep study. They can often bring their millet pillow from home and go to a lab where they will be connected to monitoring devices and computers to monitor their brain activity while they sleep. In addition to a formal sleep study, a person may be offered a Multiple Sleep Latency Test (MSLT). During one of these tests, a person will take five naps during one day and the results may be compared to the insights received during the sleep study. Often MSLT is completed the day following a sleep study.
If the doctor suspects cataplexy, they may also measure hypocretin levels. If levels are low, it may result in a diagnosis. However, there is a lot to rule out before making an official diagnosis. Receiving a narcolepsy diagnosis can take up to 9 years, and an individual may be misdiagnosed multiple times during that time period. Cataplexy is often misdiagnosed as a seizure disorder, and like other forms of narcolepsy, a cataplexy diagnosis can take years to receive.
Treating Cataplexy
There isn’t a quick fix approach or cure when it comes to treating cataplexy. Cataplexy is a lifelong sleep disorder that can be managed to reduce symptoms and occurrences. Currently, many medical professionals are approaching the condition with a combination of medication and lifestyle adjustments. The combination of the two has shown to have the best results.

Although there isn’t a magic pill that can stop all cataplectic episodes, a few medications have been shown to reduce symptoms. Research has found that antidepressants like selective serotonin uptake inhibitors (SSRIs) and Clomipramine can relieve symptoms, as well as Xyrem, which is used to treat daytime drowsiness. However, although Xyrem can reduce cataplexy symptoms, it can cause several bothersome side effects, such as drowsiness, nausea, dizziness, tremor, and involuntary urination. As a result, doctors are more likely to try antidepressants or other stimulants first.

The lifestyle changes recommended for cataplexy are centered around improving sleep quality. By improving your sleep quality and maintaining a regular sleep schedule, the symptoms can be reduced. This can be done by getting regular exercise, maintaining a healthy diet and weight, and establishing a solid bedtime routine. For example, shut off electronics at least an hour before bed and spend some time meditating on a meditation cushion. Meditation has been proven to increase sleep quality and quantity, and according to experts, getting 8 to 9 hours of sleep each night is imperative for those with cataplexy.

Individuals experiencing the symptoms of cataplexy can feel confused, anxious, and even depressed. In the United States, estimates suggest that between 135,000 and 200,000 people have narcolepsy, with just 10% having cataplexy. Its rarity and complexity means a lot of doctors and sleep experts don’t have first-hand experience diagnosing the sleep disorder, so it can take some time to receive a formal diagnosis.
If you or someone you know is experiencing any of these symptoms, they should seek medical attention right away. As the diagnosis process takes time, the sooner the sleep study is scheduled, the better. In the meantime, it is crucial to prioritize sleep. Get to bed at the same time each night and wake up the same time every morning, reduce blue light, meditate on your meditation pillow before bed and avoid naps, tobacco and alcohol during the day. By spending at least 8 hours a night on your millet pillow each night, you can take the first step in reducing your symptoms and cataplexic episodes while you wait for an official diagnosis and treatment plan.

